Signalment:
5 year old, female intact German Shepherd mix
History:
Ahsoka was transferred to the Emergency Department at Gulf Coast Veterinary Specialists from her primary veterinarian. She had a history of lethargy and decreased appetite for several days, with two episodes of vomiting and one episode of diarrhea. The owner also described a somewhat dull mentation with no seizures or tremors. Ahsoka swam in a nearby body of water right after a hurricane two weeks prior. Aside from dietary indiscretion, she had no significant previous medical history. At her primary veterinarian earlier that morning, diagnostics showed a mild leukocytosis (23.26K/uL) characterized by a mild neutrophilia (21.38k/uL), mild hyperglobulinemia (4.3 g/dL), mild hyperglycemia (140 mg/dL), and mildly elevated ALP (228 U/l). She was sedated and administered Cerenia in preparation for surgery of a suspected pyometra. She was referred to GCVS after concern for an irregular rhythm during induction.
Physical exam:
Ahsoka had a sedated mentation upon presentation. Her temperature was 102.8F, her heart rate was 140 bpm, and her respiratory rate was 28 bpm. Thoracic auscultation and abdominal palpation were unremarkable. She was ambulatory with no appreciable lameness. All peripheral lymph nodes palpated normally. She had mild dental disease, and a full coat with no evidence of ectoparasites. Her rectal exam was unremarkable.
Initial Diagnostic Tests with the emergency service:
CBC: Mild normocytic, normochromic, nonregenerative anemia (HCT 36.4%, MCV 66.1 fL, MCHC 35.7 g/dL). Mild leukocytosis (WBC 22.7 K/uL) characterized by a moderate neutrophilia (20.22K/uL), mild lymphopenia (0.98 K/uL), mild monocytosis (1.62 K/uL), and mild eosinopenia (0.04 K/uL).
Chemistry: Mild hypochloremia (105 mmol/L), moderate hyperglobulinemia (5.9), mild hyperbilirubinemia (total bilirubin 1.0 mg/dL). Otherwise unremarkable.
Snap cortisol: 4.9 ug/dL
Lactate: 1.5
PT: 14 seconds
UA: USG 1.046, pH 6.5, 2+ urine protein, no active sediment
Urine culture: No aerobic growth
Thoracic and abdominal radiographs: Small caudal vena cava associated with hypovolemia. Fluid within the bowel suggesting enteritis. Normal-sized uterine horns making pyometra unlikely. Distended urinary bladder from outflow obstruction of behavioral. Ventral sacral periosteal reaction. Incidental transitional L1.
Abdominal ultrasound: Echogenic urinary bladder debris. Mildly dilated right renal pelvis. Hyperechoic right cranial abdominal fat may be due to gastritis. Fluid filled cecum from suspect typhlitis. Incidentally septated gallbladder. Mild abdominal lymphadenomegaly most likely due to lymphoid hyperplasia.
Initial Treatment:
IVC placement, Phylyte fluid therapy, naloxone once, maropitant q24hr, Unasyn q8hr,
Added later: enrofloxacin q24hr, capromorelin q24hr, diazepam q8hr
Case Progression:
Ahsoka was hospitalized for four days. During hospitalization, she had urinary retention that responded well to diazepam. She developed a progressive anemia (HCT 29.4%) and fever (highest 103.9F), and enrofloxacin was added. Repeat thoracic radiographs showed concern for a new, faint left cranial lung pattern from superimposition or early pneumonia, and mild improvement of hypovolemia. Ahsoka showed no signs of respiratory distress while in hospital. Internal consultation with the Internal Medicine Service showed concern for mild swelling of her left and right tarsal joints, and right carpus. After improvement in her appetite and resolution of urinary retention, Ahsoka was discharged with Clavamox, Enrofloxacin, Gabapentin, and Cerenia. She presented to the GCVS Internal Medicine Service four days later for additional diagnostics, including a sedated joint tap and culture, along with more extensive infectious disease testing. On her physical exam at that time, she had difficulty rising from a lying position, with mild swelling of her right and left tarsi, and right carpus.
Additional Diagnostic Tests through the Internal Medicine Service
CBC: Moderate normocytic, normochromic, nonregenerative anemia (HCT 28.2%, MCV 64.4 fL, MCHC 36.5 g/dL), mild thrombocytopenia (124K/uL), moderate leukocytosis (WBC 27.82 K/uL) characterized by a moderate neutrophilia (24.97K/uL), and mild monocytosis (1.42 K/uL). Manual platelet count: 169,500 with moderate platelet clumping
Chemistry: Slight hypoalbuminemia (2.2 g/dL), moderate hyperglobulinemia (5.0 g/dL), mild ALP elevation (213 U/L)
Histoplasma urine antigen by EIA: Negative
Aspergillus Galactomannan EIA: Negative
Canine Comprehensive Panel (NCSU): PCR Negative for Lyme, Ehrlichia, Anaplasma, Heartworm, Apicomplexa, Bartonella, and Mycoplasma. Weakly seropositive for Rickettsia rickettsii and Babesia gibsoni, likely indicating exposure as opposed to active infection.
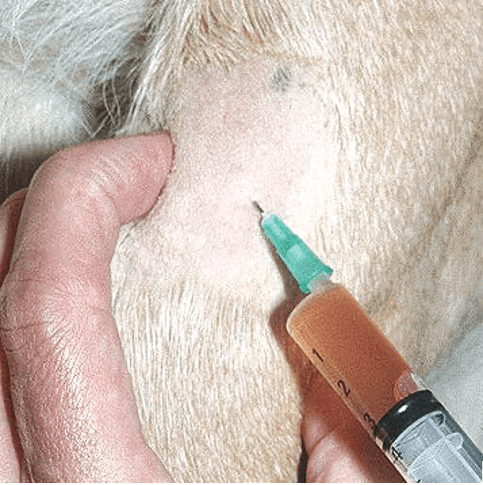
Image of arthrocentesis with aspirated fluid similar to Ahsoka’s. Grossly, aspirated joint fluid was turbid, amber colored, and less viscous. (Image obtained from Willows Veterinary Centre and Referral Service website)
Arthrocentesis cytology: Neutrophilic inflammation most consistent with immune mediated polyarthritis. No microorganisms found.
Arthrocentesis culture: No aerobic growth
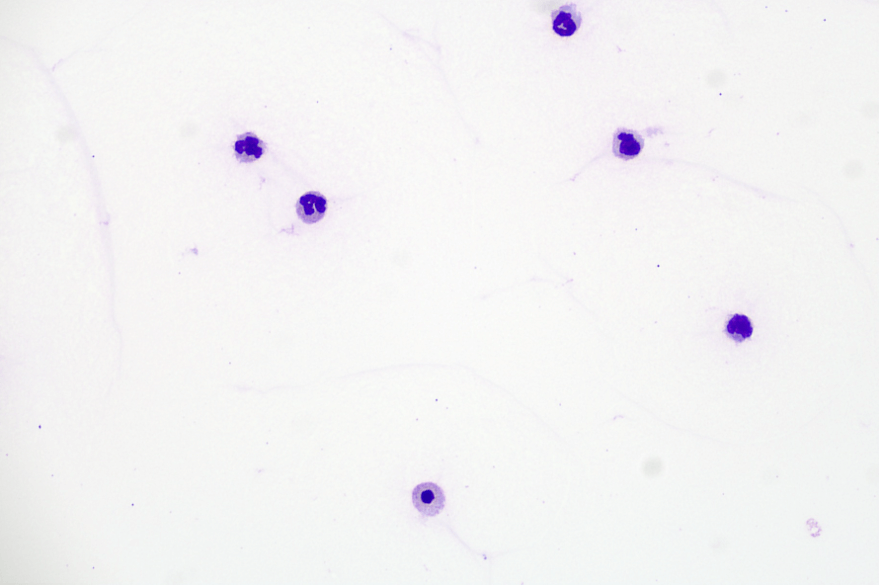
Image of cytology from the right tarsus. The slides from both locations appeared similar and consisted of lightly proteinaceous background, a relatively low number of red blood cells, and a moderately increased nucleated cell population predominated by nondegenerate neutrophils with fewer macrophages/synovial cells and rare small lymphocytes.
Follow-Up:
Ahsoka was started on prednisone (1 mg/kg/day) and leflunomide (3 mg/kg/day). She was also started on doxycycline (5 mg/kg q12hr x 2 weeks) given the weak seropositive for Rickettsia. Gabapentin was continued for the first couple of days on prednisone until comfort was achieved. A recheck is pending, but the owner reports initial clinical improvement and comfort.
Discussion:
Immune Mediated Polyarthritis (IMPA) is characterized by synovitis of two or more joints from immune complex deposition and is responsive to immunosuppressive therapy. It is often associated with systemic signs of illness including pyrexia, lethargy, and hyporexia, but can also include joint pain and swelling and reduced mobility. Any breed can be affected, with no sex predilection. Affected dogs are typically between two to seven years of age.
IMPA is classified as erosive or nonerosive, and primary (idiopathic) or secondary (reactive). Erosive IMPA causes destruction to the joint and associated bony structures, and is rare compared to nonerosive IMPA. Primary IMPA is a diagnosis of exclusion, after potential infectious and neoplastic causes are eliminated, and is the most common form. Treatment involves immunosuppressive medications, typically glucocorticoids +/- additional immunosuppressives such as azathioprine, cyclosporine, mycophenolate, or leflunomide, with the goal to taper down and attain remission. Leflunomide is the author’s preferred immunosuppressive agent for IMPA after prednisone therapy is initiated. Once clinical remission is achieved, the prednisone can be tapered in 25% dose reductions every 2 weeks unless clinical signs reoccur. The eventual goal is to maintain on once daily or every other day dosing of leflunomide. In the author’s experience, a complete medication taper often leads to recurrence of disease.
Secondary IMPA can be triggered by infectious disease, neoplasia, medications, or vaccinations. Treatment of secondary IMPA must address the underlying cause. In general, the prognosis for IMPA is fair to good, but relapse is possible. Erosive IMPA carries a poor prognosis and typically requires lifelong therapy.
In general, future vaccines are contra-indicated for patients with immune mediated disease. Where available, and accepted by law, a rabies vaccine titer could be helpful in determining if or when additional rabies vaccine doses are warranted.
Rebecca Norton, DVM, DACVIM
Karryssa Fenderson, DVM, DABVP (Canine and Feline Practice)
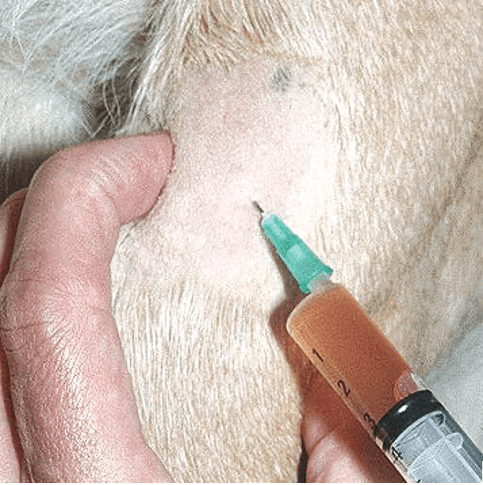 Image of arthrocentesis with aspirated fluid similar to Ahsoka’s. Grossly, aspirated joint fluid was turbid, amber colored, and less viscous. (Image obtained from Willows Veterinary Centre and Referral Service website)
Arthrocentesis cytology: Neutrophilic inflammation most consistent with immune mediated polyarthritis. No microorganisms found.
Arthrocentesis culture: No aerobic growth
Image of arthrocentesis with aspirated fluid similar to Ahsoka’s. Grossly, aspirated joint fluid was turbid, amber colored, and less viscous. (Image obtained from Willows Veterinary Centre and Referral Service website)
Arthrocentesis cytology: Neutrophilic inflammation most consistent with immune mediated polyarthritis. No microorganisms found.
Arthrocentesis culture: No aerobic growth
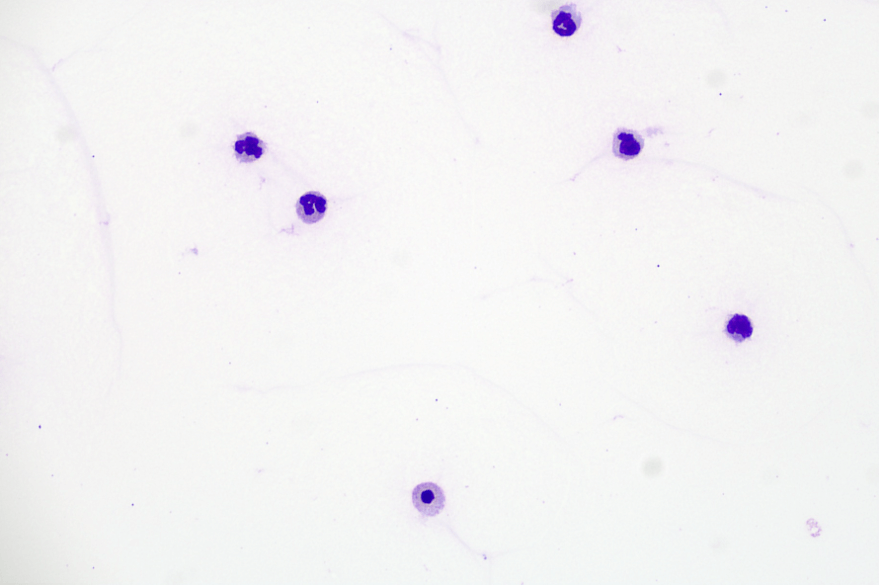 Image of cytology from the right tarsus. The slides from both locations appeared similar and consisted of lightly proteinaceous background, a relatively low number of red blood cells, and a moderately increased nucleated cell population predominated by nondegenerate neutrophils with fewer macrophages/synovial cells and rare small lymphocytes.
Image of cytology from the right tarsus. The slides from both locations appeared similar and consisted of lightly proteinaceous background, a relatively low number of red blood cells, and a moderately increased nucleated cell population predominated by nondegenerate neutrophils with fewer macrophages/synovial cells and rare small lymphocytes.